Designing and scaling up integrated mental health care for older people
May 5, 2025, 12:30 PM
Speaker: Professor Terry Yat Sang Lum (Department of Social Work and Social Administration, The University of Hong Kong)
As Hong Kong confronts the challenges of an aging population, the demographic shift has become increasingly pronounced. By the end of 2023, adults aged 60 and above accounted for 31% of the city’s population, with projections indicating that the figure will exceed 40% in the coming years. Beyond physical illnesses, over 10% of older adults experience clinical symptoms of depression, highlighting mental health as a critical yet often overlooked issue in aging societies. In response, Professor Timothy Lum and his team launched the JoyAge Mental Wellness Program in 2016, aiming to develop an accessible and sustainable mental health care model through a strategic integration of community-based efforts and primary health care systems.
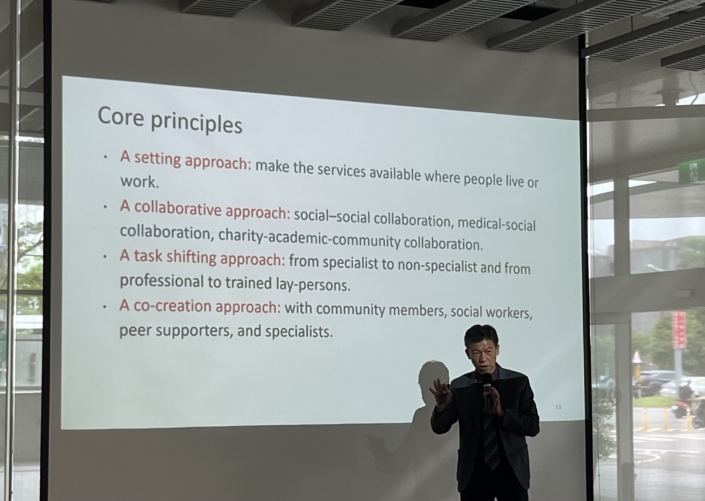
In this session, Professor Lum provided a comprehensive overview of the program’s background and implementation strategies. Grounded in the core principles of the World Health Organization’s public health framework, the JoyAge model adopts both a settings-based approach—delivering mental health support in everyday living and working environments—and a community-based approach, which empowers local residents to lead prevention and advocacy efforts. The program further embraces cross-sector collaboration, task-shifting, and co-creation, enabling social workers, clinical psychologists, health professionals, and residents to jointly develop and adapt interventions that are culturally and contextually tailored for older populations.
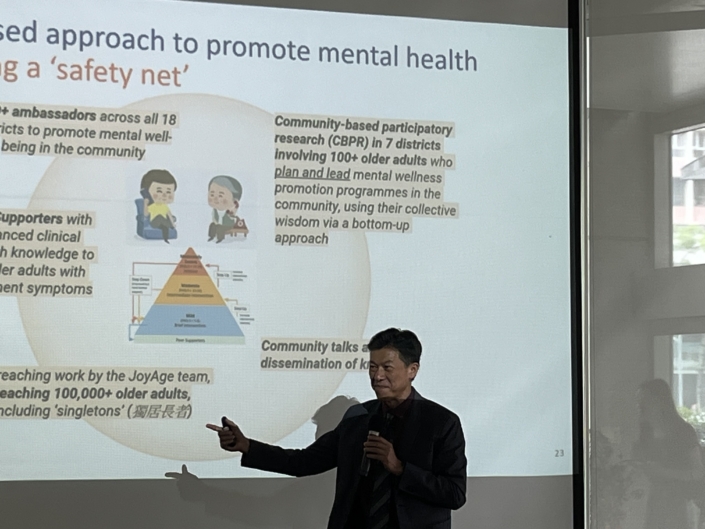
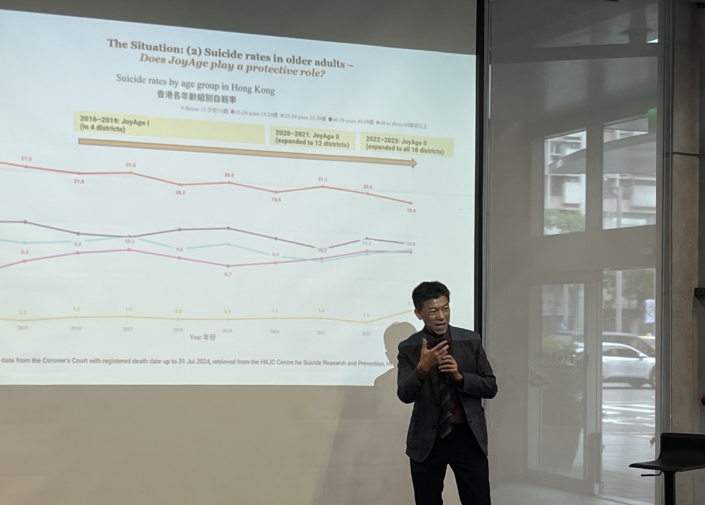
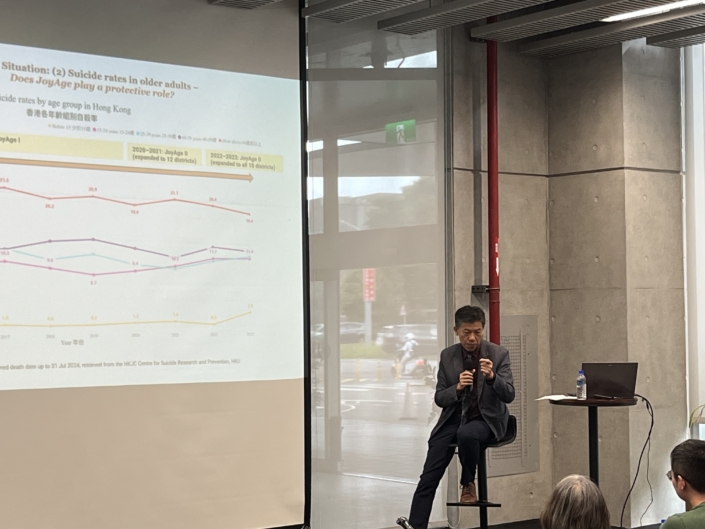
The evolution of JoyAge has unfolded in three phases. The Pilot Phase (2016–2019) introduced a stepped-care model across four districts, using quasi-experimental design to assess effectiveness. The Expansion Phase (2020–2023) scaled up the model to all 18 districts in Hong Kong, incorporating the “JoyAge Ambassadors” program to enhance mental health literacy. In the ongoing Repurpose Phase (2024–2027), JoyAge has expanded into the primary healthcare system through collaborations with District Health Centres (DHCs) and hospital networks, piloting a tri-sector integration model linking community services with general practitioners and psychiatric care.
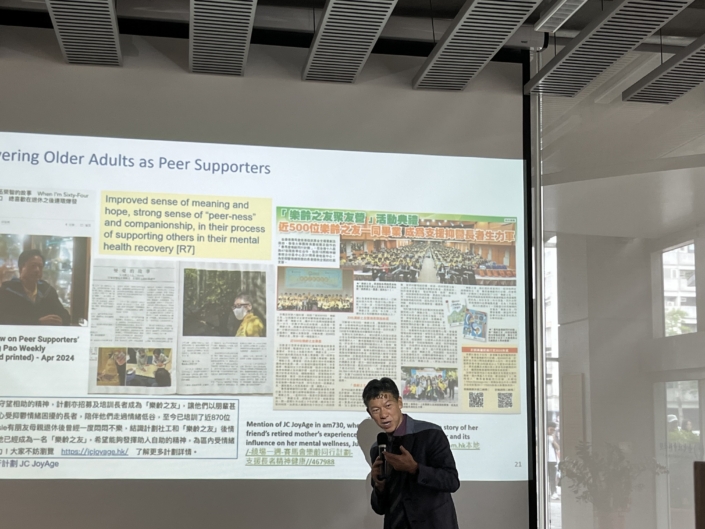
Capacity building has been a key pillar of the program. To date, over 200 professional social workers have been trained, thousands have attended workshops, and digital platforms and manuals have been developed. Notably, more than 7,000 “young-old” participants have been trained as mental health ambassadors, and over 900 peer supporters have completed intensive certification programs to provide outreach and support, collectively making over 100,000 contacts in the community. These older adults have transitioned from being service recipients to becoming vital contributors, reclaiming purpose and embodying the concept of productive aging.
Evidence-based evaluations show that the JoyAge model significantly reduces symptoms of depression and anxiety, with measurable cost-effectiveness. Compared to control groups, program participants demonstrated greater improvement in mental health outcomes and reduced healthcare utilization. In addition, JoyAge has successfully expanded the social infrastructure for mental health through innovative community engagement strategies—including peer-led support groups, public lectures, community-based participatory research (CBPR), and a crowd-sourced Wellness Map featuring nearly 300 community “healing spots.”
The program also demonstrated resilience and adaptability during the COVID-19 pandemic. The team rapidly launched phone outreach protocols, online self-help workbooks, and virtual “e-buddy” training for digital peer support. Its latest partnership with DHCs aims to create a new paradigm for integrated mental health care, linking family doctors, community social workers, and public hospital services in a unified and collaborative model.
During the Q&A session, participants raised questions about the program’s applicability to other age groups. Professor Lum noted that many mental health issues—such as loneliness, stress, and emotional exhaustion—are equally relevant to women, middle-aged caregivers, and other populations. While the model is transferrable, interventions must be adapted to meet the specific needs of different groups. He also emphasized the importance of data, policy advocacy, and seizing critical moments—such as high-profile incidents or media coverage—to mobilize institutional buy-in.
Ultimately, the JoyAge experience reminds us that mental health is not solely a clinical issue—it is a societal and structural challenge. It must be addressed not only in hospitals or clinics, but in the everyday lives of people and communities. This lecture offered an inspiring example of how older adults can become not only care recipients but also key agents of change in building a more compassionate and resilient society.
Note taken by Chia-Chia Hsu